Dec. 14 marks the one-year anniversary of the FDA’s authorization of COVID-19 vaccines for emergency use. For the first time since the pandemic began, the United States was able to have a proactive response to protecting people from the Corona virus.

“This is a day to reflect on the marvel that it is that a year after the emergence of this new virus that vaccines could be developed, tested and deployed that are remarkably effective and safe,” said Dr. Farley Verner, health authority for Waco-McLennan County Public Health District. “And now over the year that these vaccines have been in use it is likely that over 200,000 deaths and untold numbers of hospitalizations have been prevented in the United States alone.”
The local public health district received the first shipment of 200 doses of the Moderna vaccine Dec. 23, 2020, and began vaccinating first responders. Since that time, the health district has administered 64,006 doses of vaccine through mass vaccination clinics, drive-through clinics, mobile clinics, and its main clinic.
Currently, 51% of McLennan County residents ages 5 and up are fully vaccinated.
The health district offers the Johnson & Johnson, Moderna, and Pfizer vaccines Monday through Friday at the main clinic (225 W. Waco Dr.) and at mobile clinics throughout McLennan County. You can find the schedule at www.covidwaco.com/.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email the ALW team — [email protected].
By Deneece Ferrales
One-quarter of Waco residents did not see a physician for any type of routine services in 2018, the last year for which such data is available. Data from the City Health Dashboard indicates many residents do not have a primary care physician or a “medical home.”
To help more Wacoans access care, Prosper Waco’s Access to Healthcare Working Group has planned an event, “Christmas on Memorial,” 4-7 p.m. Tuesday, Dec. 7, at the Family of Faith Worship Center, 4112 Memorial Dr. The event is a partnership between the church, McLennan County Indigent Health Care, and other organizations involved with the working group. (More details below.)
The lack of access to primary health care is particularly prevalent in certain Waco ZIP codes that include many lower income and Black and Hispanic residents. The problem not only puts residents at risk but also taxes the healthcare delivery system because the lack of regular healthcare often leads to undiagnosed problems that grow bigger. This leads to urgent care, including trips to the emergency room.
The following graph illustrates the percentage of Waco/ McLennan County residents who have seen a primary care physician within a year and the bullets underneath give the percentages for the most affected ZIP codes.
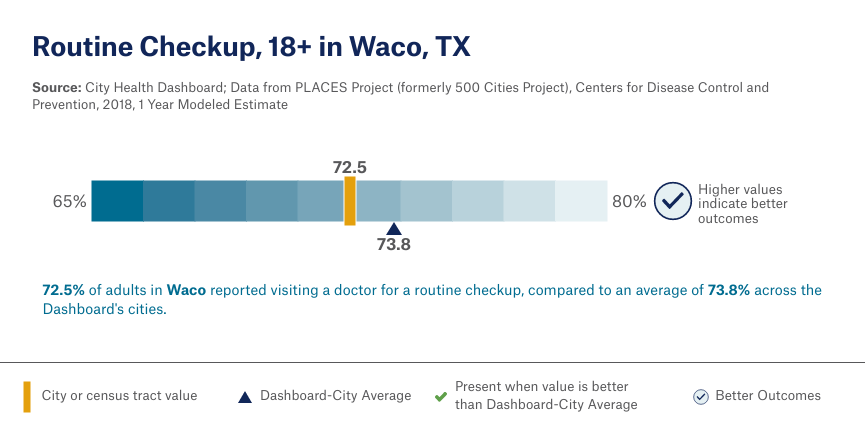
When broken down by ZIP code and census tract, the problem becomes more glaring.
- 76701, Track #1: only 66.6% of adults had a routine checkup in the past year
- 76705, Track #33: only 65.9% of adults had a routine checkup in the past year
- 76706, Track #2: only 66.5% of adults had a routine checkup in the past year
- 76798, Track #3: only 66.3% of adults had a routine checkup in the past year
Participants in “Christmas on Memorial” will have access to the following:
- Groceries for their families;
- Health screening from Ascension;
- Behavioral health screening from Heart of Texas Region MHMR,
- A COVID vaccine;
- Buy and wrap Christmas presents for kids at a reduced cost;
- Be entered into a drawing for prizes, including kids’ bicycles;
- Apply for health insurance and/or health benefits;
- Talk to a number of health agencies and providers about healthcare options and benefits; and
- A visit with Santa or play time in an on-site bounce house, along with an assortment of other kids’ activities.
The event is being held to help our community connect with healthcare resources. This event was planned by the Access to Healthcare Working Group, which is co-chaired by Heather Travers of McLennan County Indigent Healthcare and Deneece Ferrales of Prosper Waco.
For more information about this event or to sign up for a table at the event, please contact [email protected] or [email protected]. Flyers are available for distribution.
If you would like more information about the work of the Access to Healthcare Working Group, you please contact co-chairs Heather Travers or me at the emails above.
Deneece Ferrales, Ph.D., is director of health initiatives with Prosper Waco.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster.
The Waco-McLennan County Public Health District has partnered with area African American churches, the Waco NAACP, and VOICE to host a second “Shots for Souls” COVID-19 Vaccination Drive 1-4 p.m. Sunday, Nov. 14, at the Health District, 225 W. Waco Dr.
Participants can choose from the Pfizer, Moderna, or Johnson & Johnson vaccines. Adult vaccines, including boosters, and vaccines for children 5 years of age and older will be available. Lunch for the first 200 participants will be provided by the NAACP. Walk-ins are welcome and registration can be done on-line at covidwaco.com or at 254-750-5460.
“The holidays are fast approaching, and the health district is working with several organizations to get vaccines distributed just in time for the holidays,” said LaShonda Malrey-Horne, director of the health district. “The health district is collaborating with Waco NAACP, local Black churches, and VOICE Waco to offer vaccines to the East Waco community so families can enjoy the holiday season safely this year.”
Vaccination is the most effective way to slow the spread of disease and significantly decrease hospitalizations and fatalities due to COVID-19.
Waco-McLennan County Public Health District, Creative Waco, and City of Waco Parks and Recreation collaborated to create the Sidewalk Chart Art Obstacle Course Challenge. The Challenge was a community-wide project that tasked families to get outside and get creative by drawing their best sidewalk chalk obstacle course.

The Health District received multiple submissions from the community, all containing different, creative ways to get through the obstacle course such as: hopping like a bunny rabbit, spinning, doing your best touchdown dance, and jumping through lily pads like a frog.
“The goal for the challenge was to provide families with a fun way to get outside and get active, while also providing a COVID-safe activity for all to enjoy,” said Emily Green, public health education specialist for the Public Health District.
Families were asked to submit photos March 23-April 18, and winners were chosen May 3. A panel of judges representing local organizations scored the entries on creativity, obstacles within the course, and the ability for all community members to enjoy.
The winners are the Vaughn and Peebles families, the Sharma family, and the Striezel family.
The obstacle courses are now painted on sidewalks near the playground stations at Bledsoe-Miller Park (300 N. M.L.K. Jr. Blvd.), South Waco Park (2815 Speight Ave.), and Dewey Park (925 N. 9th St.). Tashita Bibles, a talented local artist, stayed true to the spirit of the kids’ original artwork, while bringing some magic of her own.
“How cool that some of the children who participated get to see their artwork come to life in City of Waco parks. It’s a reminder that everyone’s ideas can make a positive difference in our community” said Fiona Bond, executive director of Creative Waco.
Funding made possible through the Texas Healthy Communities, Texas Department of State Health Services grant.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].
By Julie Ivey
As a faculty member at Baylor, I have worked extensively helping children with autism, and I’m really excited about a current project that is innovative and free to children in the area. Our team is working one-on-one with children to improve balance, gait, behavior, and language. It’s a fun experience for the children because they do this while riding a mechanical horse.

You might have heard about the therapeutic benefits of horseback riding for children with autism; these experiences are believed to stimulate neurological connections because of the motion of the horse that the child must respond to. But not every family has access to live horses. If the mechanical horse can be effective in a clinical setting staffed by trained professionals, it can offer an excellent intervention to help children.
Through a grant from the Texas Higher Education Coordinating Board, our Baylor autism team is measuring the behavioral and language effects of riding on the MiraColt mechanical horse. Because of this funding, the experience is free to children, whose parents sign up to attend two sessions per week for 15 weeks. In fact, families who complete the study will receive $150. The project is taking place at the Baylor BRIC. Be assured that the members of our interdisciplinary team have extensive experience working with children with autism and will help the children feel comfortable in a new setting.
We are recruiting children ages 6-12 who have a diagnosis of autism and may experience motor delays. To participate, children should be able to follow simple verbal instructions and have an IQ above 80. We are accepting participants on a rolling basis this fall and spring. While the study is in its early stages, our preliminary observations are promising, and parents have said they see improvements in their children.
For a little bit more information, you can read this story from the School of Education: School of Education Autism Research Team Studies Mechanical Horse Intervention
If you think your child would be interested and would qualify, we will begin with a meet-and-greet session to show you what it is all about, meet your child, and let you explore the space.
For more information, please mail me at [email protected]! We are excited to work with children and the community on this exciting, innovative project!

Julie Ivey, Ph.D., is a clinical professor in the Baylor University School of Education.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].
By Susan Copeland
I have been working as program director of AmeriCorps Seniors RSVP for 29 years, and it has been my pleasure to serve seniors in the Heart of Texas for over 35 years. The RSVP program is sponsored by McLennan Community College and the national service agency, AmeriCorps.

Our 29th Senior Source Health and Information Fair will be 10 a.m-2:30 p.m. Friday, Sept. 17 at Richland Mall. We are excited for the opportunity to bring one-stop information and screenings to our senior population.
In a time of many concerns with the pandemic, I believe this is a chance for folks to safely visit with programs, agencies, and professionals all in one open area. Plus, participants can get their flu shots and COVID vaccines with no appointments needed.
This event can provide services such as senior living options, legal advice, benefit counseling, and so much more all in one convenient location at the mall in an open area safely spaced for COVID precautions.
AmeriCorps Seniors-RSVP has been hosting this event from its beginning and I’ve seen thousands of people gain so much from the Heath Fair. It is so satisfying to see the participants get the information they need and also enjoy the day by meeting up with friends, shopping, and learning about all the services in our area.
Caregivers get to also ask questions and collect information, and the general public always gain something from walking through the fair. It’s a win-win day for everyone and we are happy to bring it to our community.

Susan Copeland is director of the Heart of Texas RSVP program. She oversees her staff plus about 10 undergraduate and graduate student interns studying public relations, professional writing, social work, mental health, and counseling. She manages more than 50 community service projects and a force of 650 senior adult volunteers in the six-county Heart of Texas Region.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].
By Susan Menninger Krause
YMCA of Central Texas, Meals on Wheels Waco, and the City of Waco are working together to help the community take control of their health through blood pressure self-monitoring.
Nearly half of the adults in the U.S. have high blood pressure and only one in four have their blood pressure under control. High blood pressure increases the risk for heart disease and stroke, but heart attack and stroke are less likely if blood pressure is controlled. When people begin to pay attention to their blood pressure, they can better control it and improve their lives.
On Monday, Sept. 13 (11 a.m.-noon), a YMCA Healthy Heart Ambassador will begin coming to Sul Ross Senior Center to present the YMCA’s Blood Pressure Self-Monitoring program as part of the Meals on Wheels Waco programming. The program is free to eligible community members.
The YMCA’s Blood Pressure Self-Monitoring program is designed to help adults with hypertension manage and lower their blood pressure. It is a four-month program that focuses on teaching proper techniques to measure blood pressure and providing individualized support and nutrition education.
The goals of the program are to lower and manage blood pressure, increase awareness of triggers that elevate blood pressure, and help participants develop healthier eating habits. Expectations of participants are to attend office hours at Sul Ross two times a month, self-monitor blood pressure two times a month, and attend a monthly nutrition workshop.
For more information, contact Crystal Hernandez at 254.776.6612 or [email protected].

Susan Menninger Krause is manager of parks and rec facilities and programs for the City of Waco Parks and Recreation. Susan formerly was branch executive director at Waco Family YMCA.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].
By Susan Menninger Krause
Did you know that walking is one of the easiest, least expensive, most accessible ways to improve your health?
Walking will help you maintain a healthy weight, lose body fat, improve cardiovascular fitness, strengthen bones and muscles, improve balance and coordination, and increase energy. It also can help prevent or manage conditions such as heart disease, stroke, high blood pressure, cancer, and type 2 diabetes. And walking can also improve your mood, cognition, memory, and sleep.

It’s not complicated. There’s no pressure. No elaborate or pricey equipment or memberships are necessary. You control your schedule, your distance, where you go, and who you go with. Just put one foot in front of the other and join “Let’s Walk Waco” this fall.
If you’re looking to start or continue your walking journey, join the “Let’s Walk Waco” community-wide challenge. This walking challenge is sponsored by the Live Well Waco Coalition and the Waco-McLennan County Public Health District. This free eight-week program begins Sept. 20 and runs through Nov. 15. Registration begins Aug. 30.
You can create a team of your friends, neighbors, family, or co-workers or join a team and get the chance to meet and make new connections. Anyone can join, and McLennan County residents who log their miles may win prizes along the way.
For information on how to register, create, or join a team, visit our website. There you will also find information about community center parks and indoor walking opportunities, City parks and trails, frequently asked questions, and other helpful tips and resources. Come join the fun and “Let’s Walk Waco.”

Susan Menninger Krause is manager of parks and rec facilities and programs for the City of Waco Parks and Recreation. Susan formerly was branch executive director at Waco Family YMCA. Before coming to Waco, she worked 16 years at Greater Joliet Area YMCA near Chicago. Susan holds a bachelor’s degree in English from the University of Texas at Dallas and a master’s degree in kinesiology from the University of North Texas. She and her husband, Ken, have two sons, Zachary and Tyler, both are in college.
Act Locally Waco also has an informal group of walkers called Waco Walks. There is more information on our Waco Walks web page.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].
Meraki Medical Associates LLP will begin offering COVID-19 vaccinations Friday, Aug. 20, at 1001 Dunbar Street in East Waco. The opening is planned in conjunction with August being National Immunization Awareness Month.

CEO Sophia Strother formed Meraki “to create access and awareness for communities of color in the East Waco,” she said. Meraki is Greek for doing something with soul, creativity, and love. “It’s important to always put something of yourself into what you’re doing, whatever it may be. We are a starting point for the sustained health of our community. We will be known for our compassion and ability to provide services to everyone we encounter with meraki.”
Strother is passionate about helping communities of color fight against COVID. After having over 10 family members directly affected by the virus, she decided she needed to take action. Partnering with Living Word Church of God in Christ, Meraki is set to open its clinic Aug. 20 to provide community-focused health awareness on the importance of vaccine-preventable diseases. It will provide vaccination clinics and educational opportunities statewide that will target underserved communities and special populations.
Meraki is at 1001 Dunbar St., Waco. This building has housed Living Word Church of God in Christ, Meals on Wheels, and Community Food Pantry for all of 20 years. Meraki believes “every person deserves an opportunity to be given a health experience that inspires them and enhances their quality of life. The team hopes to partner with other faith-based organizations, community organizations and corporations to administer vaccinations to individuals 16 years and older.” Sophia is passionate about helping others through faith, knowledge, and resources.
Aug. 20 Events at Meraki
11 a.m. – 11:30 a.m. – Tour
11:30am – noon – Press Conference
Noon – 2 p.m. – Vaccination Clinic
Strother also owns a logistics company and was recently featured on HGTV’s “40 Year Old Property Virgin.” Connect with Sophia online here.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].
By Suzii Paynter March
There is no avoiding a crisis; chaos can come in all sizes. Everyday good people are faced with unimaginable bad luck, disasters, break downs, unexplainable confusion, desperation and violence. But none of these should be the last word on anyone’s life.
The worst thing that happens to you should not define you. But all too often, a crisis and the chaos it brings, changes everything and every relationship in sight. What if every crisis ended up on your doorstep?

Waco needs a crisis hub. A crisis hub is a place that is a combined resource center that can help streamline decisions, bolster support, provide a smooth hand off, and share the load to help people in crisis avoid the chaos that can destroy themselves and their families.
Right now, mental health professionals, medical personnel, City of Waco, and McLennan County leaders are working toward building the right team to respond to overwhelming crises and build a place for Waco to have a crisis hub. Responding to the kinds of personal crises that can bring harm to self and others and finding the way out of chaos takes a team.
Through the leadership of the Prosper Waco working group, the Behavioral Health Leadership Team, the Board of MHMR, and the advice of other communities who have also tackled this problem, Waco is retooling to minimize the chaos that wreaks havoc on friends, family, and neighbors. Bringing existing resources together matters, and it multiplies the effectiveness of intervention.
The number of people in crisis and the intensity of the crises grow month by month. One frustrated man in crisis described Waco as a pinball machine – “I know I need help, but all I can do is bounce around town or be drunk or violent. Can’t somebody catch me on the bounce. I know I need help?”
Teams in a crisis hub can function together to avoid duplication of efforts; they can minimize missed opportunities and promote persistence; they can support each other in the very hard work of helping people climb out of chaos and find hope. A crisis hub team can find steps toward solutions JUST because they are together and can bring many talents to bear all at once. Concentrating services helps the person in crisis and it helps sustain the strength of the professionals working together, too.
When is the sum greater than its parts? When a small group of caring, talented people step in together to tackle chaos and come out the other side with hope. I would not know what to do if the crisis were on my doorstep, but I can be part of the solution by supporting the team that is building the Waco Crisis Hub.

Suzii Paynter March is chief executive officer of Prosper Waco.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email Ferrell Foster at [email protected].